2Department of Gastroenterology, Samsun Training and Research Hospital, Samsun, Türkiye
3Department of Gastroenterology, University of Health Sciences, Prof. Dr. Cemil Taşcıoğlu City Hospital, Istanbul, Türkiye.
Abstract
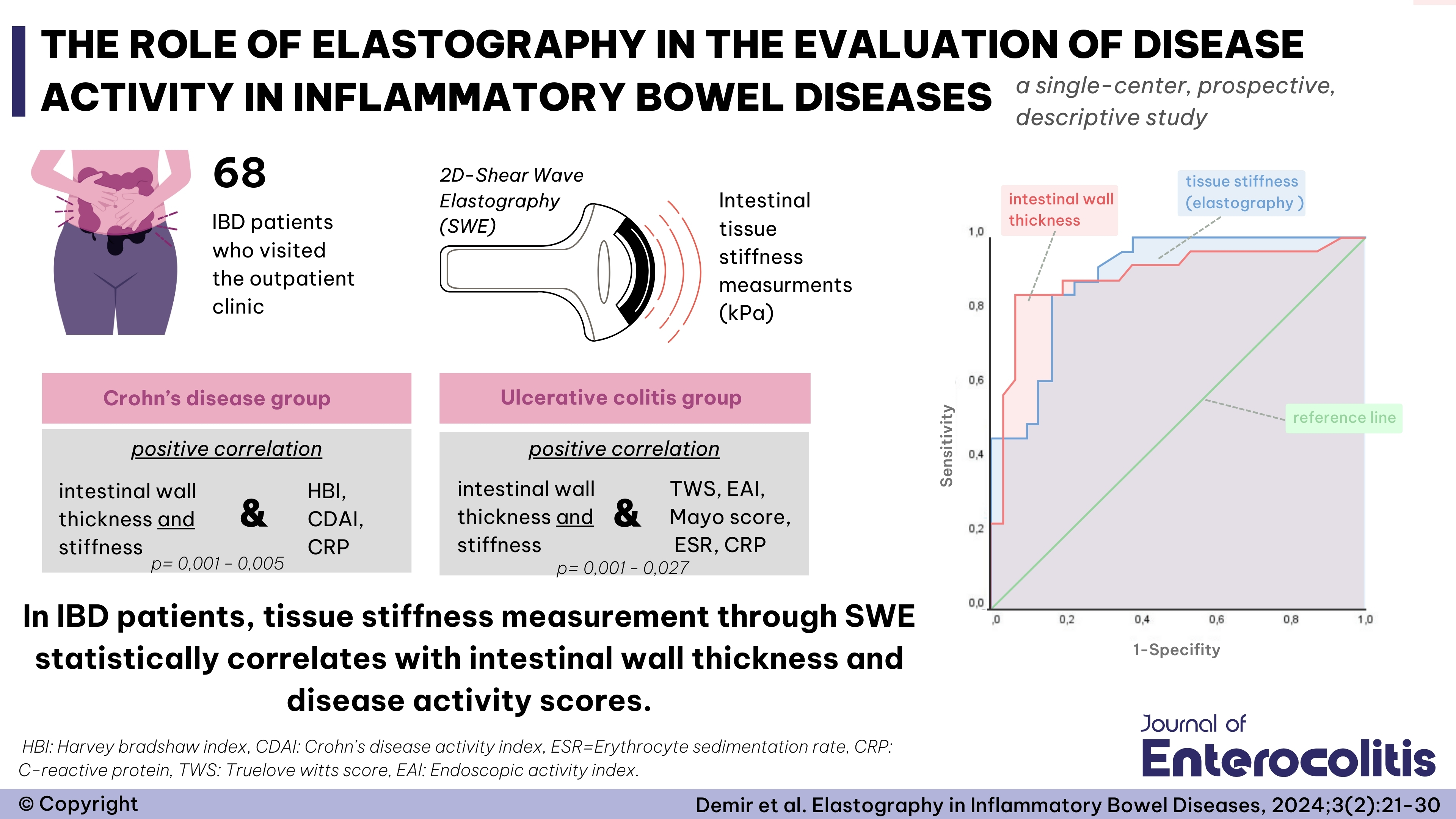
Objective: Inflammatory Bowel Disease (IBD), encompassing Crohn’s Disease (CD) and Ulcerative Colitis (UC), is a chronic immune-mediated condition associated with systemic inflammation that may increase the risk of cardiovascular disease (CVD). This study aimed to investigate the utility of novel, accessible inflammatory and atherogenic biomarkers—Plasma Atherogenic Index (PAI), Monocyte-to-HDL Ratio (MHO), and Systemic Immune-Inflammation Index (SII)—in assessing cardiovascular risk and disease activity in IBD patients compared to healthy controls. We also evaluated the association of these markers with Abdominal Aortic Calcification (AAC), a surrogate for subclinical atherosclerosis.
Methods: This retrospective, single-center study included 99 IBD patients (40 with CD, 59 with UC) and 70 healthy controls evaluated between January 2017 and April 2023. Demographic, clinical, and laboratory data were collected from patient files. PAI (log[Triglycerides/HDL-C]), MHO (Monocyte/HDL-C), and SII ([Platelet × Neutrophil]/Lymphocyte) were calculated. Disease activity was assessed using the Crohn’s Disease Activity Index (CDAI) for CD and the Mayo score for UC. AAC was assessed in patients with available abdominal computed tomography (CT) scans. Statistical analyses included group comparisons and Receiver Operating Characteristic (ROC) curve analyses.
Results: IBD patients demonstrated significantly higher levels of PAI, MHO, SII, and Neutrophil-to-Lymphocyte Ratio (NLR) compared to the healthy control group (p < 0.05 for all). Within the IBD cohort, patients with active disease exhibited significantly higher SII and NLR values compared to those in remission. However, PAI levels did not differ significantly between active and inactive disease states. Of the 63 patients evaluated with CT, 40 (63.5%) had AAC. Patients with AAC had significantly higher levels of CRP, NLR, SII, MHO, and PAI compared to those without AAC (p < 0.01 for all). ROC analysis identified PAI and MHO as strong predictors of AAC presence.
Conclusion: The novel, easily calculable biomarkers PAI, MHO, and SII are significantly elevated in patients with IBD, suggesting a heightened pro-inflammatory and pro-atherogenic state. The strong association of these markers with AAC reinforces their potential utility in identifying subclinical atherosclerosis and increased cardiovascular risk in this patient population. These findings suggest that routine calculation of these indices could aid in cardiovascular risk stratification for IBD patients, although further validation through large-scale, prospective studies is warranted.


 Burcu Ağırbaş Çelen1
Burcu Ağırbaş Çelen1