Abstract
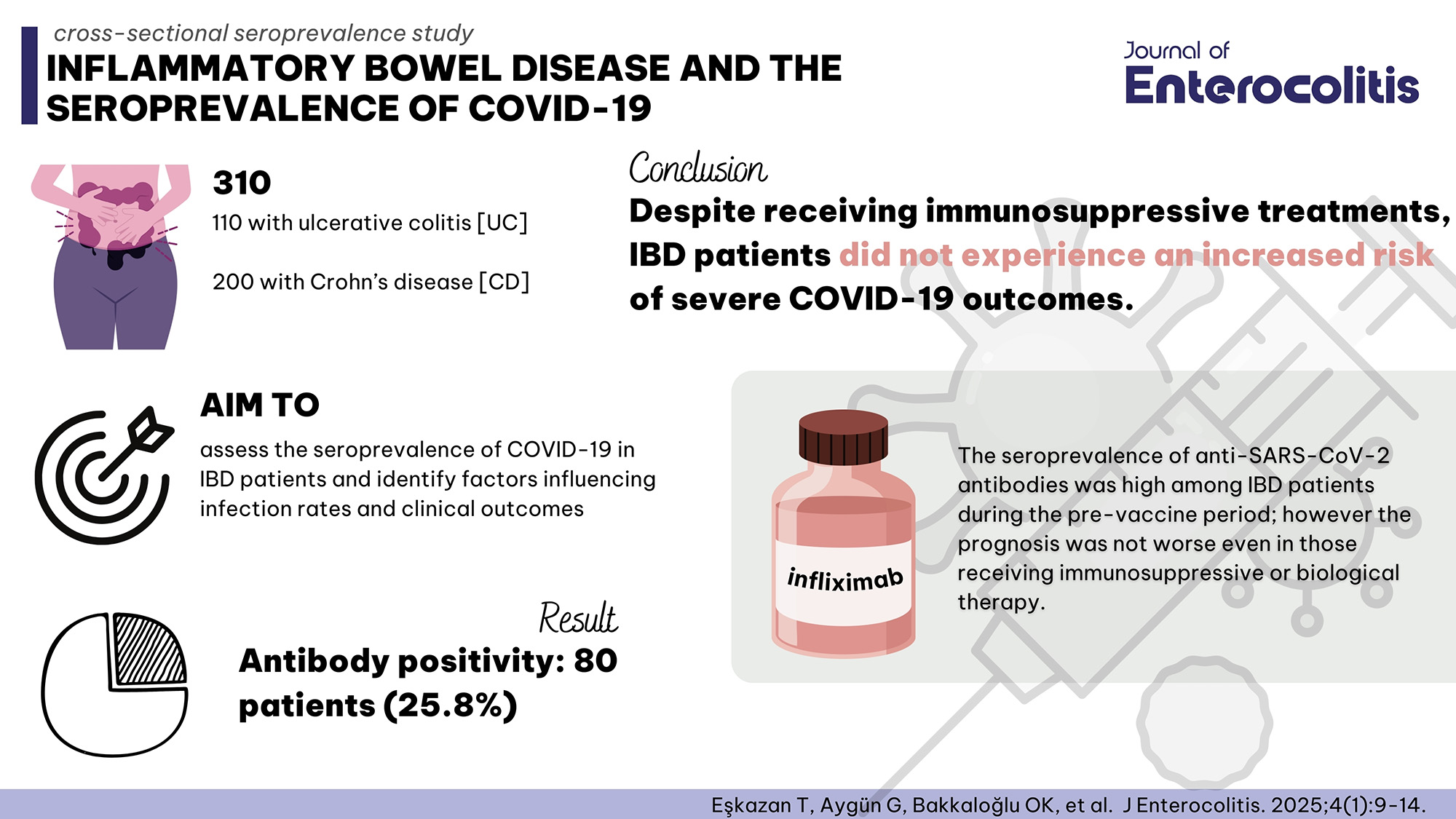
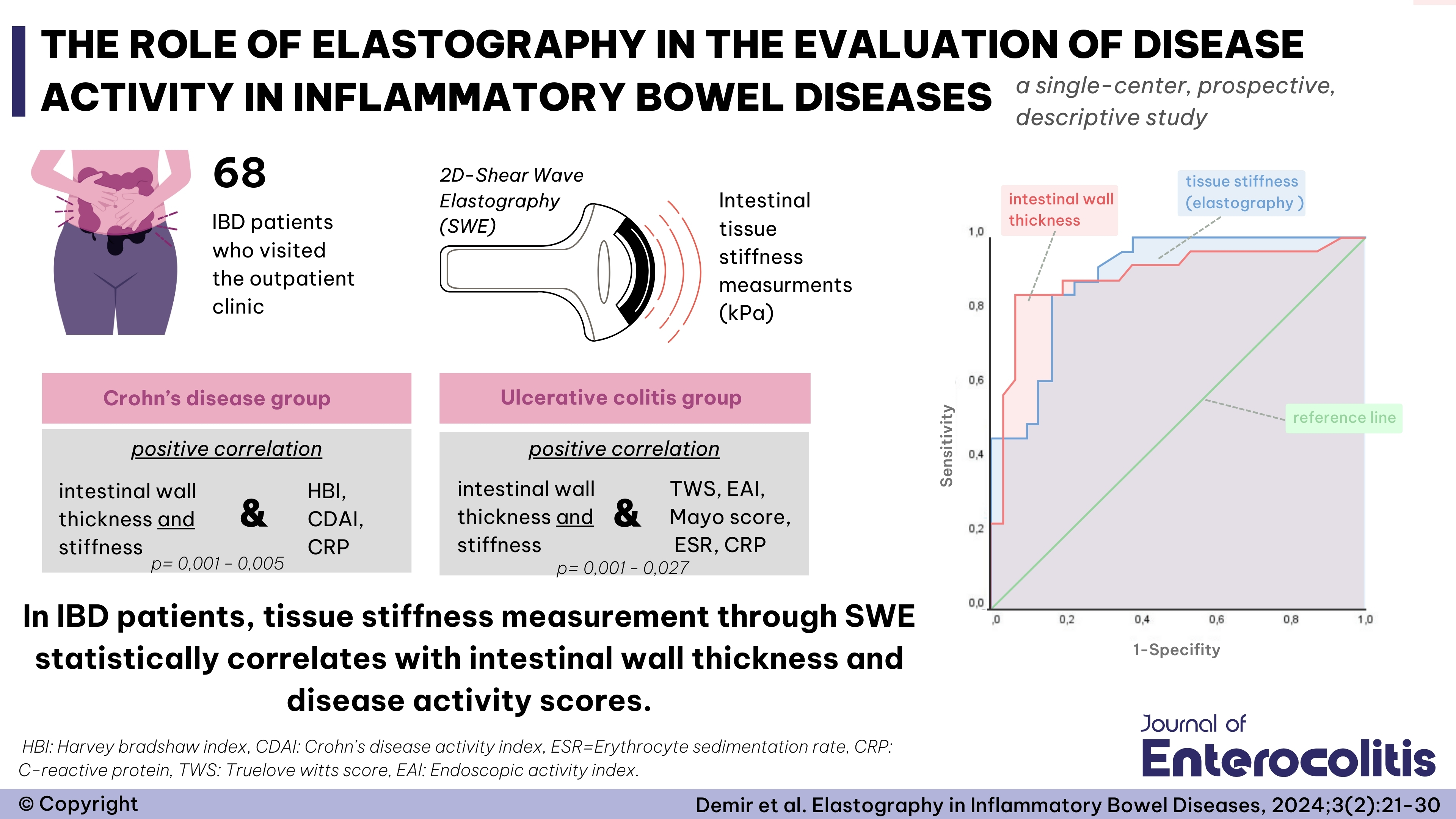
The goal in managing inflammatory bowel disease (IBD) is to achieve both clinical and endoscopic remission. Additionally, improving patients’ quality of life is a primary objective. With recent innovations in treatment and the expansion of therapeutic options, histological remission has also become a target. In treatment planning, factors such as the patient’s current clinical status, age, comorbidities, and previous treatment history are crucial considerations. All available treatments require attention to specific precautions, contraindications, and parameters that need regular monitoring. Although TNF-α inhibitors are highly effective in treating IBD, they increase the risk of complications such as latent tuberculosis (TB) reactivation and opportunistic infections. Therefore, screening for latent TB is conducted before initiating anti-TNF therapy, and TB prophylaxis is administered to patients who require it. Mesalazine, one of the oldest drugs used in IBD treatment, has been associated with acute interstitial nephritis, making it essential to monitor renal function in patients receiving this medication. Azathioprine, commonly used for its immunosuppressive properties, has been linked to side effects such as cytopenia, hepatotoxicity, and acute pancreatitis. Consequently, patients on azathioprine should be closely monitored for these adverse reactions. Treatment strategies for IBD should be individualized, taking into account patients’ clinical status, socio-demographic characteristics, and comorbidities. Regular follow-up and monitoring for adverse drug reactions are critical components of care for patients undergoing treatment.


 Tugce Eskazan1
Tugce Eskazan1