2Department of Gastroenterology, Gazi Universitesi Faculty of Medicine, Ankara, Türkiye
3Department of Gastroenterology, Aksaray University Training and Research Hospital, Aksaray, Türkiye
4Department of Radiology, Gazi Universitesi Faculty of Medicine, Ankara, Türkiye
5Department of Public Health, Gazi Universitesi Faculty of Medicine, Ankara, Türkiye
6Department of Medical Biochemistry, Gazi Universitesi Faculty of Medicine, Ankara, Türkiye
Abstract
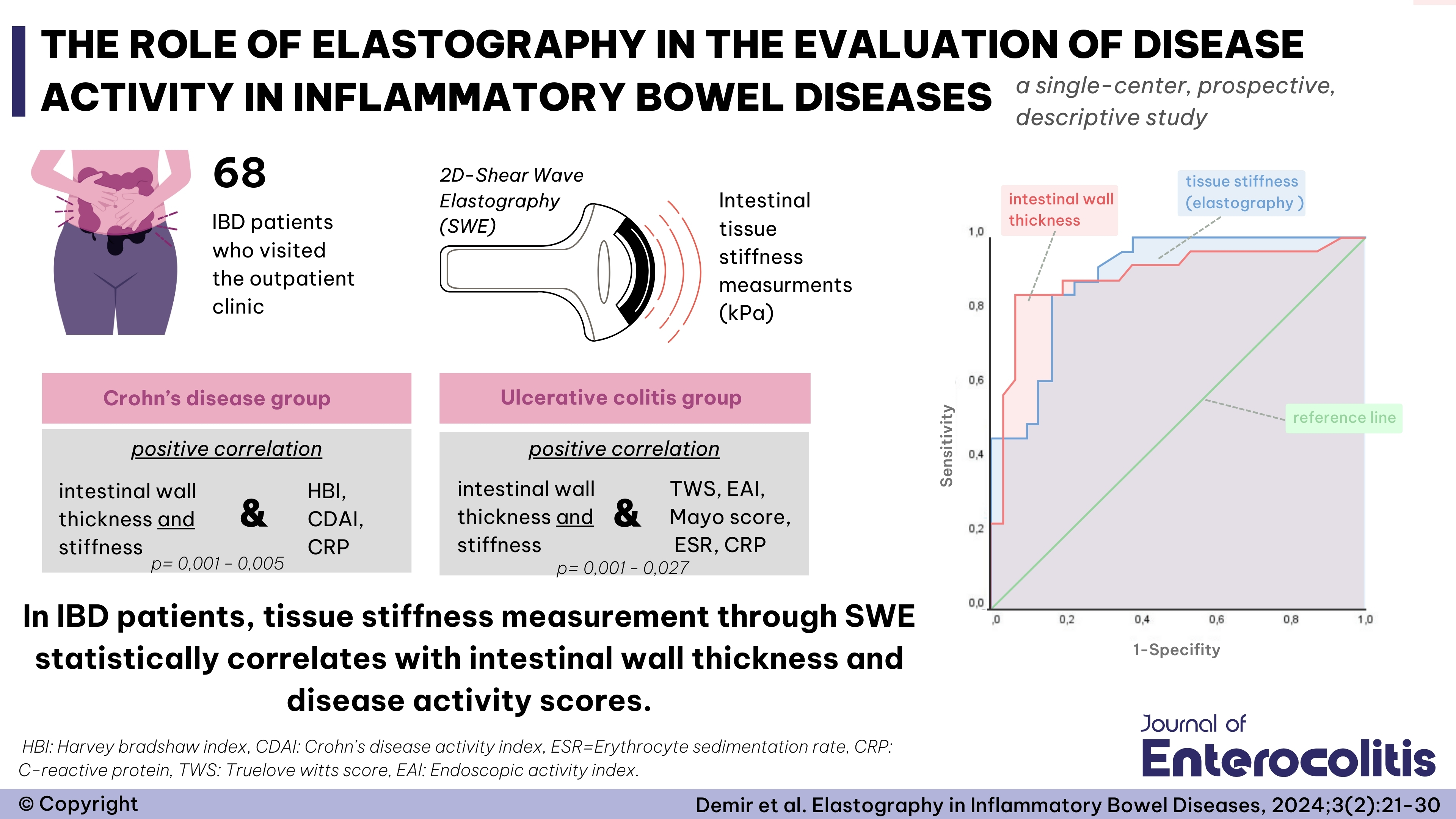
Objective: Inflammatory bowel disease (IBD) encompasses chronic inflammation of the intestinal mucosa, including ulcerative colitis and Crohn’s disease. Various parameters, scoring systems, and imaging methods are used to evaluate disease activity and treatment outcomes. Ultrasound elastography is a non-invasive, radiation-free method that assesses intestinal fibrosis and activity. This study aimed to evaluate the efficacy of ultrasound elastography in assessing disease activity in IBD patients, both in remission and active phases.
Methods: This prospective descriptive study included 38 patients with ulcerative colitis and 22 with Crohn’s disease. Disease activity in ulcerative colitis patients was evaluated using the Mayo score, Truelove-Witts score, and Endoscopic Activity Index (EAI), while Crohn’s disease patients were assessed using the Crohn’s Disease Activity Index (CDAI) and Harvey Bradshaw Index (HBI). Patients were categorized according to disease activity. An experienced radiologist used 2D shear wave elastography (SWE) to measure intestinal stiffness in kilopascals (kPa). Statistical analysis was conducted using the Kolmogorov-Smirnov and Mann-Whitney U tests. The ROC curve and Youden Index were applied to determine the cut-off value for diagnostic accuracy.
Results: The mean age of the patients was 43.4±14.5 years. A statistically significant positive correlation was found between intestinal wall thickness and HBI, CDAI, ESR, and CRP in the Crohn’s disease group (P<0.001, P<0.001, P=0.005, P=0.001, respectively). In the ulcerative colitis group, a statistically significant correlation was also observed between intestinal wall thickness and TWS, Mayo score, EAI, ESR, and CRP (P<0.001, P<0.001, P<0.001, P=0.027, P<0.001, respectively). Additionally, a statistically significant correlation was found between tissue stiffness and HBI, CDAI, and CRP in Crohn’s disease, and between tissue stiffness and TWS, Mayo score, EAI, ESR, and CRP in ulcerative colitis.
Conclusion: The study revealed a statistically significant correlation between stiffness measurements (kPa) obtained through 2D-SWE, intestinal wall thickness measured by transabdominal ultrasound, and disease activity scores. 2D-SWE is a valuable tool that can complement other clinical indicators in evaluating disease activity in IBD.


 Emre Demir1
Emre Demir1