2Department of Pathology, Istanbul University, Faculty of Medicine, İstanbul, Türkiye
3Department of Radiology Istanbul University, Faculty of Medicine, İstanbul, Türkiye
Abstract
Eosinophilic gastrointestinal diseases include diseases that develop as a result of eosinophilic infiltration of the entire gastrointestinal tract from the esophagus to the anus and can manifest with different presentations. Histopathological evaluation is important in diagnosis. Steroid is the most effective agent in the treatment, and the duration should be determined according to the place of involvement of the disease and the clinical picture.
INTRODUCTION
Eosinophilic gastroenteritis (EG) is a disease characterized by eosinophilic infiltration of the gastrointestinal tract in the absence of secondary causes and is often found in patients with a history of allergic disorders. Eosinophilic gastroenteritis can affect any age, with a slightly male predominance.1 Patients often present with a wide range of signs and symptoms such as abdominal pain, nausea, vomiting, dysphagia, diarrhea, and even more serious manifestations such as intestinal obstruction or perforation.2,3 We reported 3 cases with esophageal, stomach, and intestinal involvement.
CASE 1
A 73-year-old woman presented with intermittent abdominal pain and nausea for 2 years. She had watery diarrhea and subileus attacks intermittently, especially last 1 month. She has hypertension, allergic asthma, and a history of cholecystectomy.
Physical examination showed abdominal distension. There was no organomegaly. Laboratory tests on admission revealed eosinophilia (eosinophil: 2300/mm3, normal range: 0-600/mm3) and normochromic normocytic anemia.
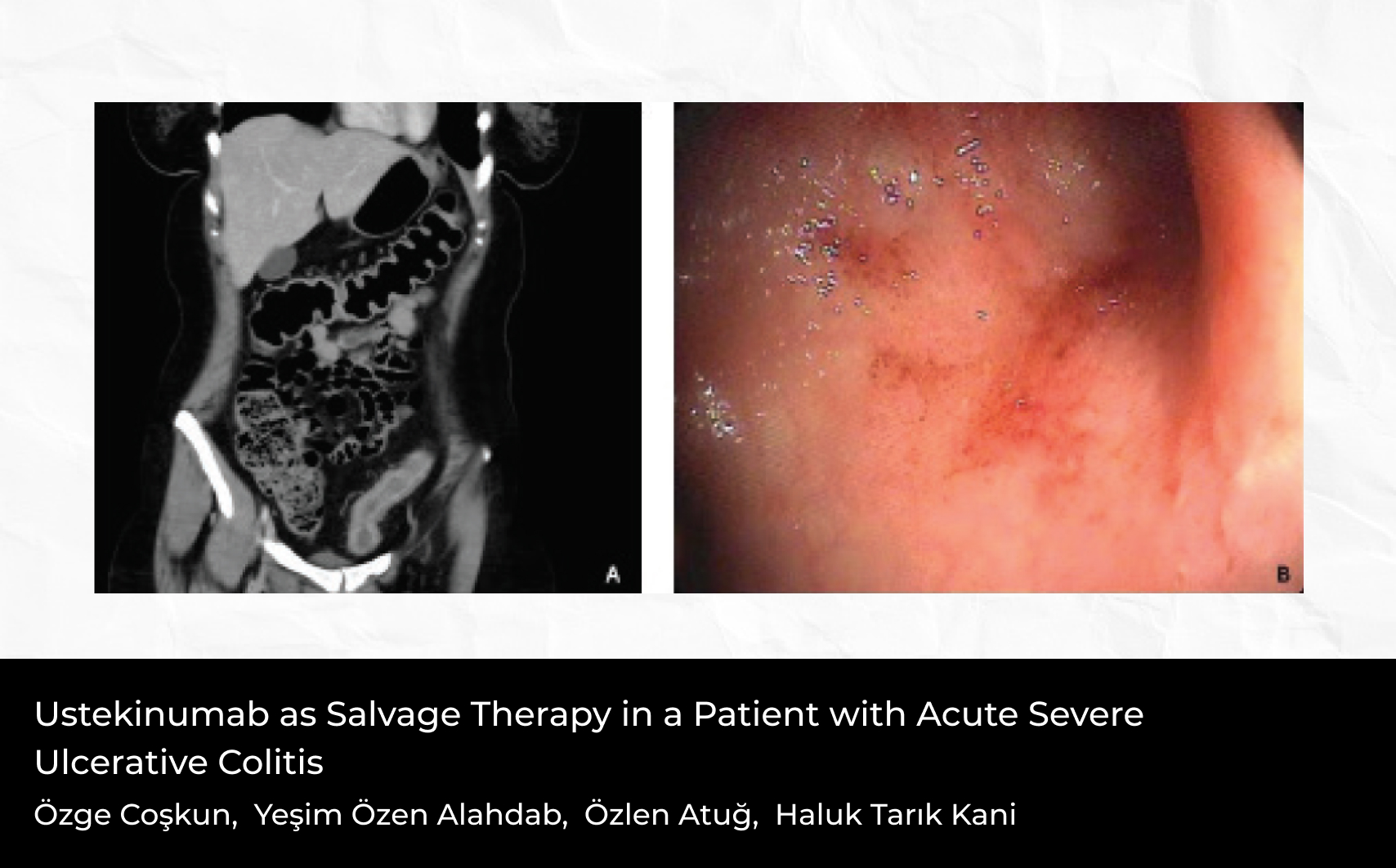
Serum thyroid, kidney, electrolytes, liver, coagulation studies tests, immunoglobulin (Ig) E level, and acute phase reactants were normal. Stool examinations were negative for parasites, ova, and other common pathogens. Viral serologies were negative. Peripheral smear showed dense eosinophil cells and no atypical cells. Abdominal computed tomography (CT) showed increased wall thickness and fluid around the jejunum and middle ileal segments (Figure 1).
Positron emission tomography-computed tomography showed focal activity involvement in the jejunum.
She underwent esoph agoga strod uoden oscop y (EGD) and colonoscopy. There was a serrated polyp on the descendant colon and its biopsy was tubulovillous adenoma. Then, she underwent doubleballoon enteroscopy and we detected ulcers in the jejunum (Figure 2).
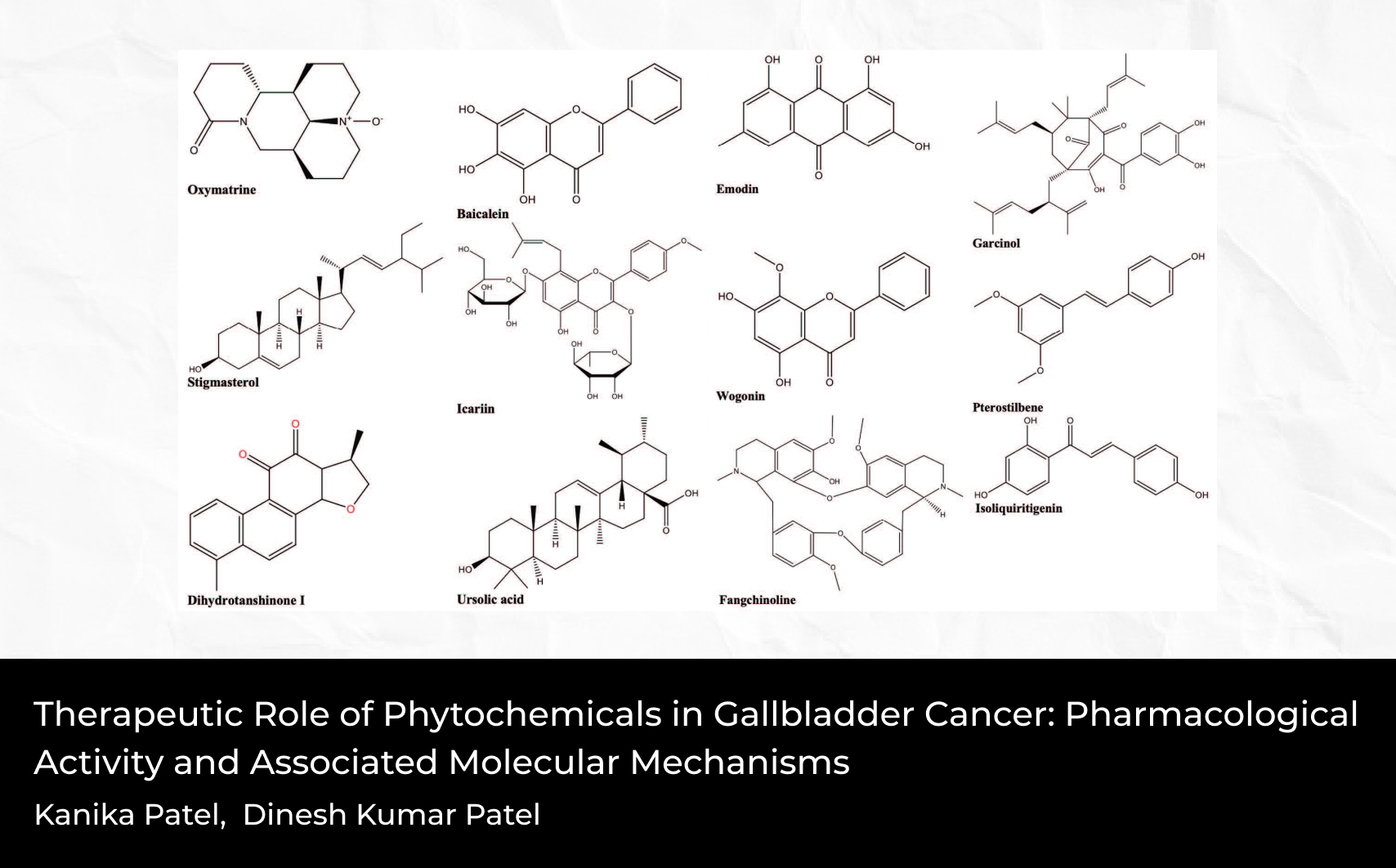
In the microscopic examination, mucosal ulceration with intense eosinophilia and eosinophilic infiltration filling the entire lamina propria was seen in the jejunum and duodenum. Eosinophilic cryptitis was observed in some areas. In the jejunum, dense eosinophilic infiltration forming an eosinophilic abscess in the entire submucosa was detected (Figures 3 and 4).
Since there was no pathological finding related to Crohn's, the ileum was normal endoscopically, the ulcer appearance was not compatible with Crohn's, and the patient had asthma in the anamnesis and eosinophilia in the peripheral blood, the patient was accepted as eosinophilic enteritis and methylprednisolone treatment was started with a tapering scheme. Over time, the dose of methylprednisolone was reduced and discontinued, and the patient is being followed up without complaints in the 1 year of treatment.
CASE 2
A 37-year-old woman has dust and drug allergy. A ptotic stomach was detected in the passage graph performed for 2 years due to dyspepsia and intermittent dysphagia. In the examinations performed on the recurrence of dyspeptic complaints after symptomatic treatment, physical examination revealed clepotage. There was no organomegaly. Laboratory tests on admission revealed eosinophilia (eosinophil: 5200/mm3, normal range: 0-600/mm3).
Serum thyroid, kidney, electrolytes, liver, coagulation studies tests, and acute phase reactants were normal. Stool examinations were negative for parasites, ova, and other common pathogens. Total IgE level was 127 IU/mL (N < 100 IU/mL). Viral serologies were negative.
Peripheral smear showed dense eosinophil cells and no atypical cells.
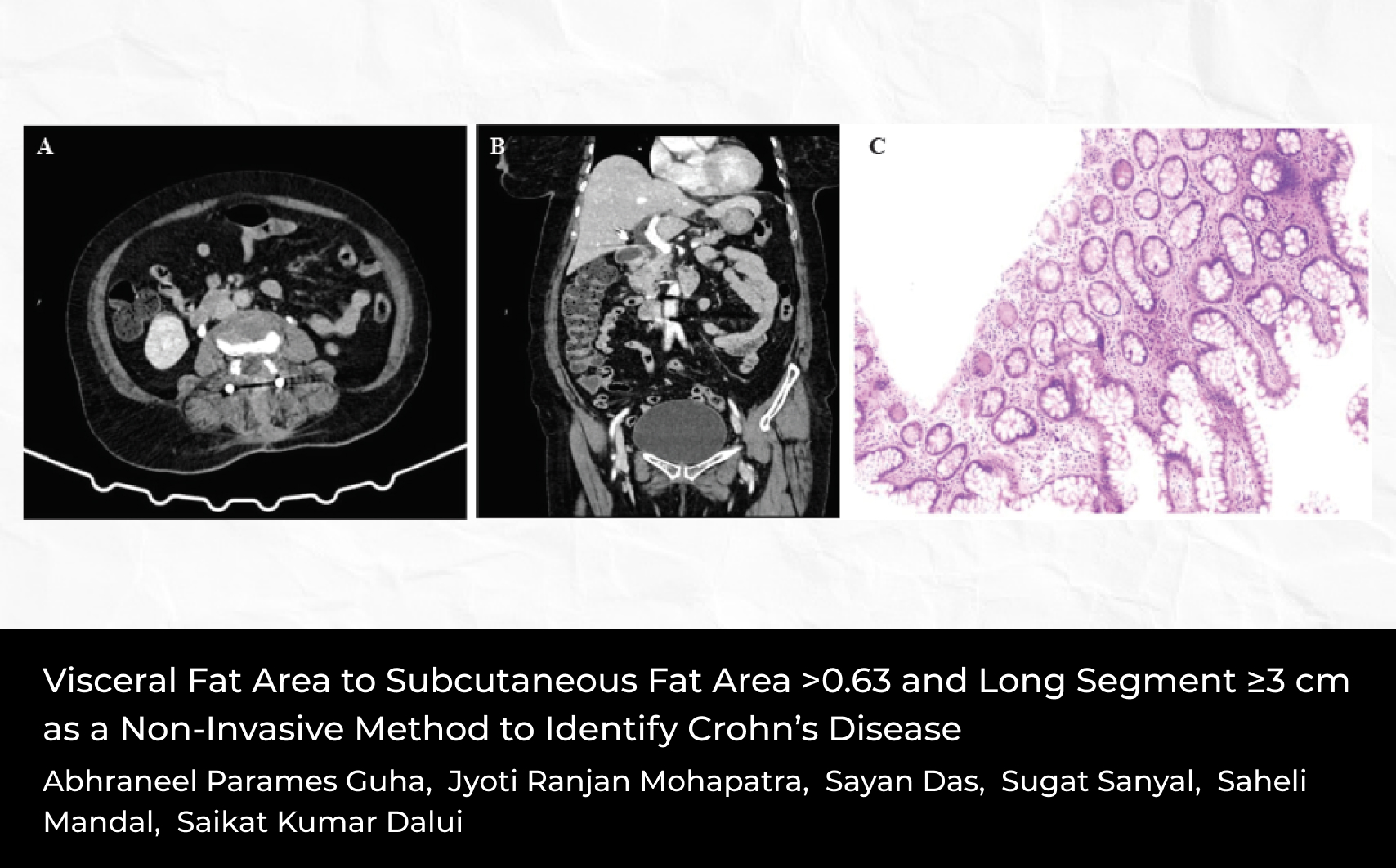
Diffuse wall thickness increase was detected in the distal esophagus, antrum, proximal and middle jejunal segments, and distal and terminal ileal segments in thorax and abdominal CT (Figure 5).
Gastrointestinal system was examined by colonoscopy, gastroscopy, and oral enteroscopy. There was no major pathology in the EGD and colonic mucosa was erythematous in places and there was a diminutive polyp in the ascended colon, also.
Microscopic examination revealed eosinophilrich infiltration in lamina propria of the duodenum and gastric mucosa. In the duodenum, numerous eosinophils within the muscularis mucosa were seen (Figure 6).
Eosinophilic enteritis was diagnosed, and methylprednisolone treatment was started. Over time, the dose of methylprednisolone was reduced and discontinued, and the patient is being followed up without complaints at the 10th month of treatment.
CASE 3
Our patient is a 22-years-old man. In the examinations performed for dysphagia 3 years ago, hemogram and biochemical examinations were found to be normal. The EGD examination did not reveal any features; however, after >25/high power field (HPF), eosinophils were detected in the pathology of biopsy samples taken from her esophagus. He was diagnosed with eosinophilic esophagitis and methylprednisolone treatment was started with a tapering scheme. The patient received intermittent methylprednisolone treatment for 3 years, during the control EGD 3 years later, and esophageal laceration occurred during the passage of the endoscope through the esophagus wall and the possibility of perforation developed. Thereupon, hemoclips were placed on the lesion area and the patient was followed up. No other complications occurred in the follow-up.
DISCUSSION
Eosinophilic gastrointestinal diseases occur as a result of excessive eosinophil infiltration in the gastrointestinal tract, although the pathogenesis has not been fully explained. Eosinophilic gastrointestinal diseases include the diseases that develop as a result of eosinophilic infiltration of the entire gastrointestinal tract from the esophagus to the anus (eosinophilic esophagitis, eosinophilic gastritis, eosinophilic enteritis, eosinophilic colitis).4 In this article, we reported 3 cases with different clinical presentations. The first case presented with subileus attacks and the second with signs of gastroparesis. In the last case, the risk of perforation occurred during endoscopic control, possibly due to disease-related fragility. The first 2 cases had peripheral eosinophilia and a history of allergy.
Differential diagnosis is important for this condition. These diseases can be primary as well as secondary to infection, drug reaction, vasculitis, neoplasia, and hypersensitivity. In addition, an increase in eosinophils can be seen in some conditions such as gastroesophageal reflux disease, inflammatory bowel diseases, functional dyspepsia, and celiac disease. We excluded all of these secondary causes by immunologic, endoscopic, radiologic, and pathologic examinations.
Eosinophilic gastrointestinal diseases are relatively more common in women than in men.5 The clinical presentation may vary according to the involved tissue and the depth of involvement.6 Patients may present with symptoms of abdominal pain, chest pain, nausea, vomiting, dyspepsia, and dysphagia.7 Rarely, as in our case, eosinophilic gastrointestinal diseases may also present with ileus, especially in the involvement of the muscular layer, as our first case. In serosal involvement, eosinophilic acid, peritonitis, and even perforation (in our third case, there was a perforating risk) may occur in patients.5 Diagnosis of eosinophilic gastrointestinal diseases is made by demonstrating eosinophilic infiltration in the gastrointestinal tract with endoscopic biopsy and excluding secondary causes in the presence of related symptoms. There is usually a normal appearance with endoscopy, but erythema, ulcer, nodularity, and mucosal fragility can also be detected.8 We detected ulcers in the jejunum by double-balloon enteroscopy in our first case. Peripheral eosinophilia and serum total IgE elevation can also be seen in patients, as in our second case.9 An increase in wall thickness can be detected in cross-sectional imaging.
Diet modification, corticosteroids, leukotriene receptor antagonists, proton pump inhibitors, and biological agents have a place in the treatment of the disease. If secondary causes can be identified, it is important to eliminate them.4 Although corticosteroids form the basis of treatment, combined treatments may be considered if no response is obtained. Corticosteroids are usually started at a dose of 0.5-1 mg/kg and administered as induction therapy for 2 weeks. Afterward, the treatment is continued with a dose reduction scheme of 6-8 weeks.10 Intermittent corticosteroid therapy was also used in our cases.
In conclusion, eosinophilic gastroenteritis may present with different presentations. Gastrointestinal system involvement may not always be seen with endoscopic findings. A biopsy is absolutely necessary for suspected patients.


 Zülal İstemihan1
Zülal İstemihan1